
How exercise affects your eyes
Regular exercise has long been recognized as a way to improve overall health and well-being. Exercise can reduce the risk

Regular exercise has long been recognized as a way to improve overall health and well-being. Exercise can reduce the risk
It might come off astounding at how contrasting vision and eye health could be between men and women. Take for
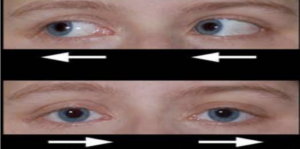
Nystagmus is an eye condition where the eyes move rapidly and are unable to control. The areas of the brain