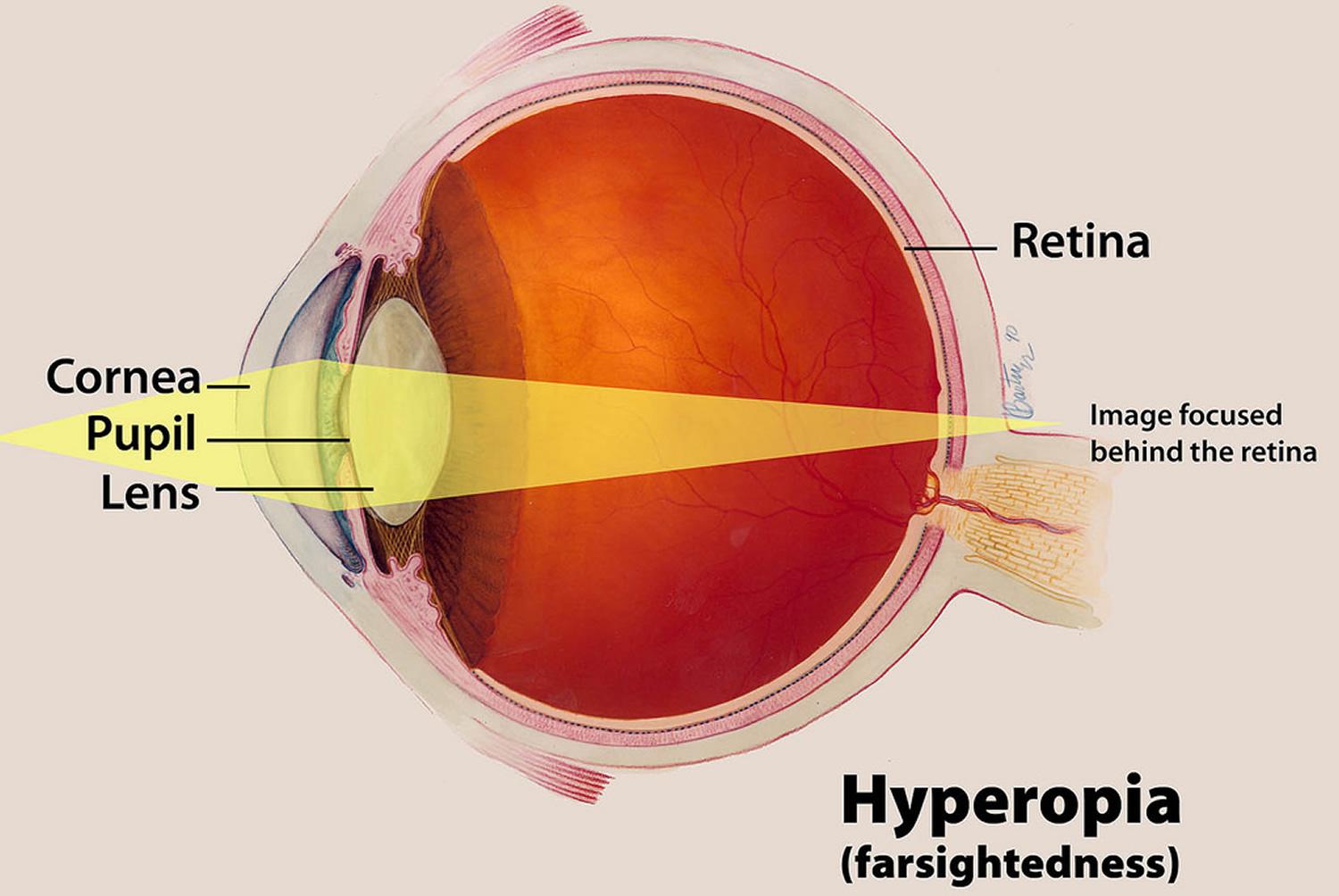
Hyperopia is also known as far-sightedness. It is a common type of refractive error that occurs when the light is focused behind the retina of the eye. Hyperopia affects near vision more, which means that distant objects can be seen more clearly than near objects.
There is a possibility that a combination of refractive errors can occur concurrently. For an example, hyperopia and astigmatism can occur in the same eye, or one eye can be short-sighted while the other is far-sighted. Hyperopia (rabun dekat in Malay) should not be confused with presbyopia (rabun tua in Malay) as they are not the same. Presbyopia is age-related and occurs when changes in the eye is less able to accommodate, and losing its ability to focus on close-up prints or objects. Hyperopia can occur at any age while presbyopia usually occurs over the age of 40.
Symptoms of Hyperopia/Far-sightedness
- Difficulty in seeing close-up objects
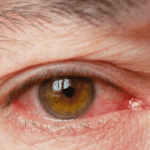
- Eye strain or eye tiredness
- Headaches, especially when doing close-up tasks
- Blurred vision
- Squinting
- Fatigue
These symptoms tend to be more obvious after doing some near work such as reading, computer use, mobile phone activity and so on. The symptoms can vary, depending on the prescription. For individuals with mild farsightedness, the symptoms may not be so noticeable. Regular eye examinations are important to ensure that your vision is optimal. Individuals with moderate or severe hyperopia, may notice their vision is blurred for near and distant objects.
Causes of Hyperopia
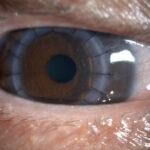
Hyperopia occurs when images are focused behind the retina. From an anatomical standpoint, it is seen in eyes that are shorter. The cornea also plays a major role. If the cornea is too flat or less curved than normal, it might also cause images to fall behind the retina.
There is a genetic component involved with hyperopia, so most hyperopic individuals are born with a preponderance for it. Studies show the refractive errors are primarily influenced by multiple genes, so if a direct family member such as a parent or sibling is hyperopic, there is an increased likelihood of developing hyperopia. External factors such as lifestyle and diet may also influence changes.
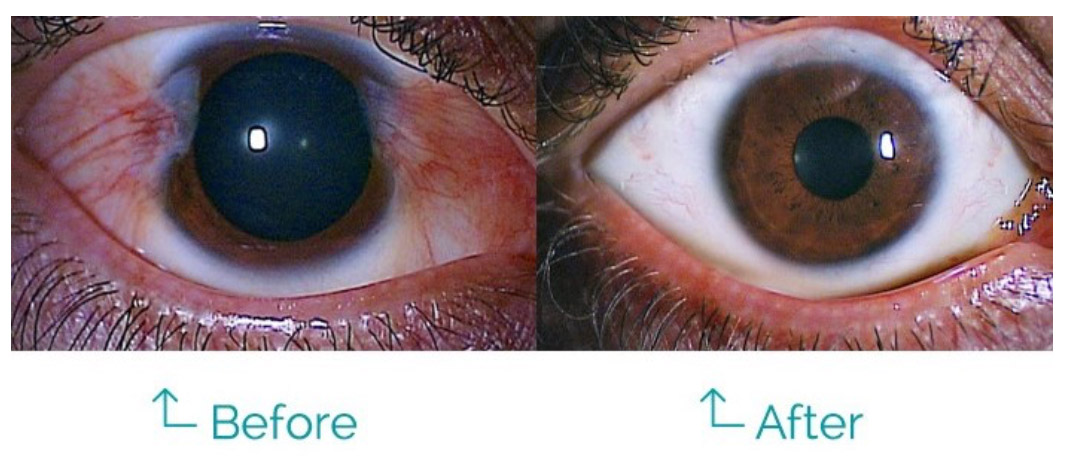
Treatment
In young individuals, treatment may not be necessary because the natural lenses in the eyes are flexible enough to accommodate and compensate for mild to moderate degrees of hyperopia. The common management for hyperopic individuals is with glasses or contact lenses
- Glasses -This is the most direct, simple and safe way to improve vision caused by hyperopia. There are different types of lenses such as those for single vision, bifocal lenses and progressive multifocal lenses.
- Contact lenses. Soft clear lenses are worn on the eyes. They are available in a variety of materials and designs such as soft and Rigid Gas Permeable (RGP) lenses. They are available in monofocal or multifocal designs. There are contact lenses that correct hyperopia and astigmatism as well.
For individuals who prefer to be glasses-free and not rely on any glasses or contact lenses:
Orthokeratology lens (Ortho-K):
Ortho-K is the fitting of a customized rigid gas permeable (RGP) lens that is worn overnight. While the individual sleeps with the RGP lenses on, the lenses will gently reshape the front surface of the eye known as cornea. Clear vision can be achieved the following day upon removal of the lenses. Ortho-K can lenses only correct low degrees of hyperopia.
Refractive Lens Exchange (Cataract surgery):
This procedure involves removing the natural lens in the eye and implanting an artificial lens that corrects the hyperopia. This procedure usually applies to individuals who are above 40 years old, around the time when cataracts may start to develop and presbyopia sets in. Following a refractive lens exchange, individuals will not require cataract surgery in the future.
Laser Refractive Surgery
Laser surgery is done by reshaping the curvature of the cornea using a low energy laser machine. It is a good option for patients with hyperopia including PRK, TransPRK, and LASIK. TransPRK is a no touch ‘LASIK’ and bladeless treatment which is able to treat up to +6.00D of hyperopia.











 Bagaimana cara menyembuhkan sembelit?
Bagaimana cara menyembuhkan sembelit?


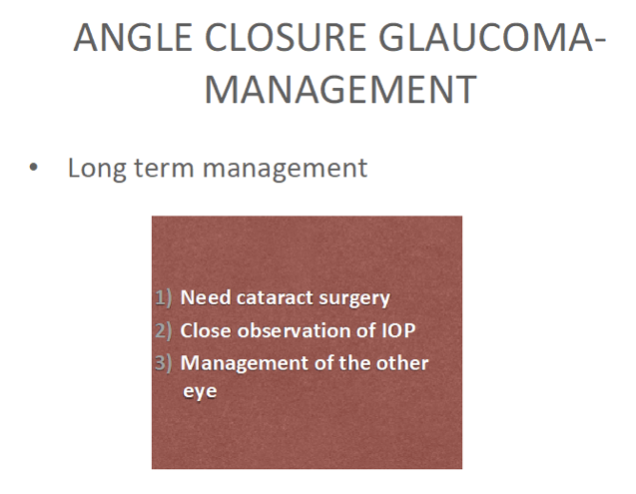
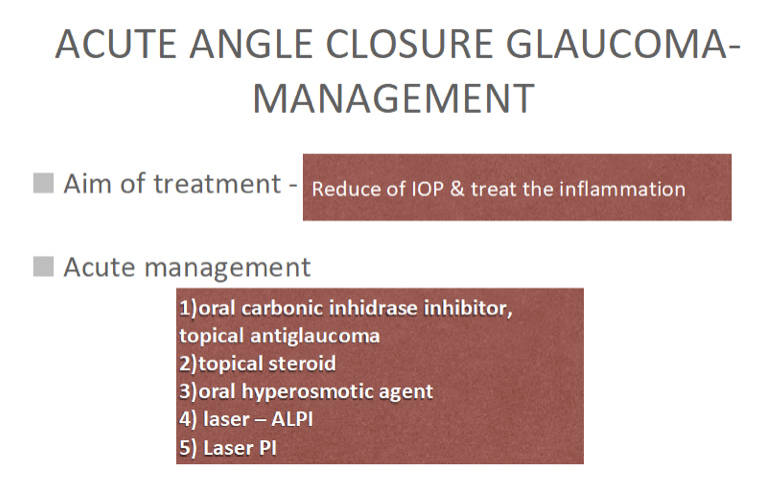 Once the IOP is controlled with laser treatment and anti-glaucoma medications and the affected eye has stabilized, there is a need to plan for cataract surgery in the future. All these are done to reduce and prevent irreversible damage to the optic nerve and thus maintain quality of life.
Once the IOP is controlled with laser treatment and anti-glaucoma medications and the affected eye has stabilized, there is a need to plan for cataract surgery in the future. All these are done to reduce and prevent irreversible damage to the optic nerve and thus maintain quality of life.